By Nicholas Fox, Nolan Fox, Thomas Das, Roger S. Blumenthal, Ethan Tumarkin
A high level of low-density lipoprotein cholesterol (LDL-C) is a major contributor to the development of atherosclerosis, the leading cause of cardiovascular disease. Managing cholesterol levels is a focal point of current treatments for CVD prevention.
This article summarizes the current information about managing lipid levels by incorporating recent advances in treatment and risk assessment with the 2018 Guideline on the Management of Blood Cholesterol by the American College of Cardiology and
the American Heart Association (ACC-AHA).
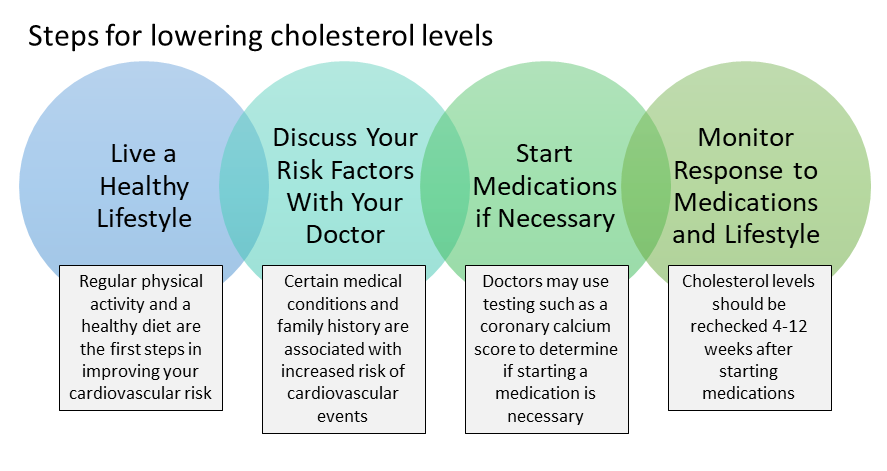
Lifestyle Management
Adhering to a healthy lifestyle remains the most important action in the management of blood serum cholesterol levels. Every individual, regardless of family history or current health status, can benefit greatly from lifestyle management and significantly
reduce their risk for coronary heart disease and stroke. Lifestyle management encompasses many aspects of an individual’s everyday life, including diet, exercise and behavioral habits.
LDL Cholesterol Level and Risk
While LDL-C levels are linked to increased development of atherosclerotic cardiovascular disease, not everyone with high cholesterol will have a heart attack or stroke. In recent years, treatment of people with high cholesterol or triglycerides (blood
fats) now focuses on those at greatest risk for cardiovascular disease. As cardiovascular risk increases, so does the absolute benefit of lowering LDL-C levels.
Current recommendations include specific percentage reductions in LDL-C
levels (either >30% or > 50%) based on an individual’s absolute risk. LDL-C thresholds (such as > 70 mg/dL in very high risk or > 100 mg/dL in those with probable familial hypercholesterolemia with baseline LDL-C > 190 mg/dL)
are also used to decide whether adding non-statin therapies (ezetimibe or a PCSK9 inhibitor) to statin therapy is appropriate for individuals at high risk of atherosclerotic cardiovascular disease.
Shared Decision Making
The ACC-AHA guidelines emphasize a shared decision-making process when determining a treatment course for a patient with high cholesterol. This includes a review of a patient’s major cardiovascular disease risk factors, as well as the patient’s
estimated level of risk within the next 10 years and possibly over the next 30 years. The benefits of both a heart-healthy lifestyle and lipid-lowering therapy should be discussed, as well as a review of any concerns the patient has about starting
a medication.
Lipid Management in Primary Prevention
The 2018 guidelines recommend using the ASCVD risk estimator plus to estimate 10-year ASCVD risk. The risk calculator is intended
for adults 40-75 years of age, who do not have diabetes, and whose LDL-C levels are between 70 and 190 mg/dL. Patients can be categorized by their risk of disease at 10 years as: low (<5%), borderline (5% to 7.5%), intermediate (7.5% to 20%) or
high (>20%).
For low-risk individuals, reinforcement of lifestyle changes is generally sufficient. For intermediate or high-risk individuals, starting a moderate or high-intensity statin and lifestyle changes are suggested to decrease
LDL-C levels by 30% or 50% respectively. Also, certain risk-enhancing factors (such as a family history of early heart disease, prediabetes, an underlying inflammatory condition such as rheumatoid arthritis or lupus) can justify starting statin treatment
in patients with borderline or intermediate risk.
Among patients at borderline to intermediate risk at 10 years (5% to <20%), the net benefit of lipid-lowering medication may still be uncertain in a patient not inclined to start on a
statin. The U.S. guidelines suggest a coronary-artery calcium test (CAC test) can be done to better assess risk, and to help decide if a statin treatment would be beneficial in these individuals. For a patient with a CAC score >100, or at >75th
percentile for their age, a statin is recommended. Additionally, a statin should be considered with any degree of CAC. In patients with a CAC score of 0, treatment with a statin may be withheld, unless they smoke cigarettes.
Estimation
of lifetime cardiovascular risk may be considered in patients 20-59 years old to start discussions about the importance of maintaining a healthy lifestyle. The decision to use statins in patients older than 75 should be made taking into consideration
the patient’s other conditions, life expectancy, and preferences.
In summary, the combination of risk-enhancing factors and a CAC score assessment can allow for a personalized treatment decision regarding lipid management and
primary ASCVD prevention.
Primary Prevention in Severe Hypercholesterolemia or Diabetes
For individuals with severe primary hypercholesterolemia (LDL-C level ≥190 mg/dL), a high-intensity statin (or maximum dose tolerated) is recommended to reduce lifetime risk, regardless of their estimated 10-year risk of ASCVD. If LDL-C levels remain
≥100 mg/dL, additional treatment with ezetimibe, a PCSK9 inhibitor, or both, should be considered.
Patients with diabetes who are 40 to 75 years old and have LDL-C levels ≥70 mg/dL should generally initiate treatment with a moderate-intensity
statin regardless of their 10-year risk of ASCVD. It is reasonable to prescribe a high-intensity statin to patients with diabetes and a higher risk of ASCVD due to multiple risk factors, to reduce LDL-C levels by >50%
Lipid Management in Secondary Prevention
All individuals with clinical atherosclerotic cardiovascular disease who are 75 years old or younger should aim to reduce their LDL cholesterol level by at least 50% by using a statin at the maximum tolerated dose.
For very high-risk patients, ezetimibe can be added to the maximum tolerated statin if LDL-C levels are > 70 mg/dL. If LDL-C levels remain at or above 70 mg/dL, a PCSK9 inhibitor can be added. Individuals 75 or older may still begin or continue either
moderate or high-intensity statins. But their statin dose may need to be reduced if they are at risk of harmful effects.
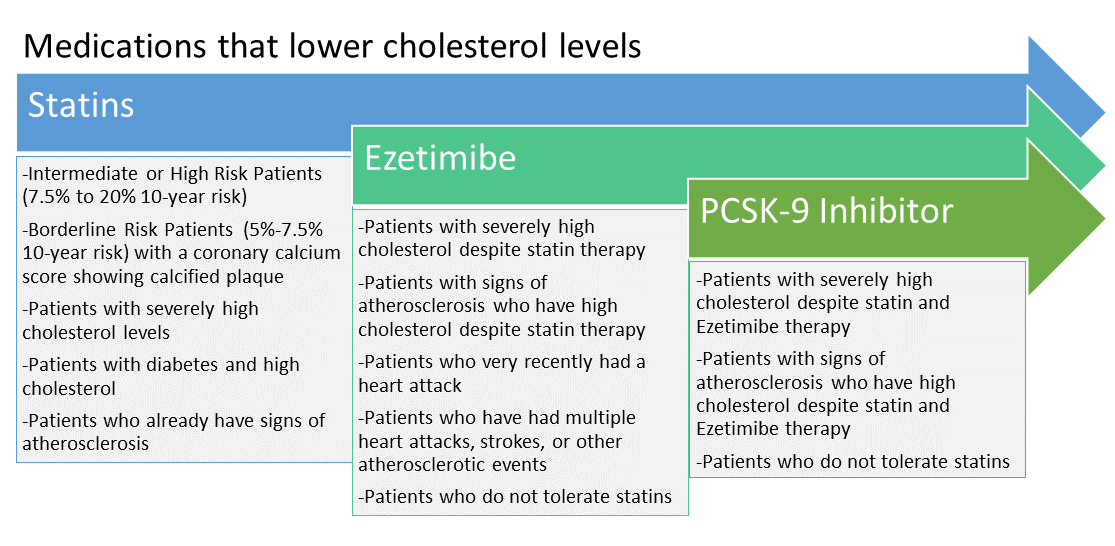
Overview of Lipid-Lowering Drugs
Statins: First-line treatments for lowering LDL-C levels. The benefits from statin therapy outweigh the risks for most patients indicated for treatment, and statins are most effective when taken long-term.
Ezetimibe: A second-line treatment for lowering LDL-C levels, which is often prescribed in addition to a statin, is often used in patients with severe hypercholesterolemia, those who have insufficient reduction in LDL-C levels when taking the maximum tolerated
statin dose, and those who experience side effects with statins.
PCSK9 Inhibitors: Are used for high-risk patients who have harmful reactions to statins or who have not had adequate reduction in LDL-C levels while
taking the maximum statin dose in addition to ezetimibe.
Omega-3 Fatty Acids: May be used to reduce the rate of major cardiovascular events in patients with hypertriglyceridemia and low HDL levels, despite controlled
LDL levels. Recently, a high dose of a type of purified fish oil (EPA) was approved to reduce cardiovascular risk.
Other Agents: Emergence of the mentioned treatments has led to less use of older agents such as fibrates,
niacin and bile-acid sequestrants.
Emerging Approaches that have not yet been approved for clinical use:
- Inclisiran has shown the potential to reduce PCSK9 synthesis and LDL-C levels and requires dosing just 2-3 times a year.
- Bempedoic Acid reduces cholesterol synthesis and is less likely to cause effects on muscles occasionally experienced with statins.
- AKCEA-APO(a)-LRx is a drug that has shown promise in early trials and may be able to reduce lipoprotein(a) levels by up to 90% without harmful effects.
Additional Considerations
The 2018 ACC-AHA guidelines suggest measuring lipid levels every 4 to 12 weeks after starting or adjusting statin therapy. Later, measuring lipid levels every 3 to 12 months is recommended.
Statin intolerance
is defined as the inability to receive two or more different statin treatments. Approach statin intolerance in patients through a review of drug-drug interactions and related health conditions. Then trying a different statin (often begun every other
day) is recommended.
Conclusions
Blood cholesterol level management is central to the prevention of heart attacks and strokes. Talking about cardiovascular risk is called for with all patients. Lifestyle changes targeted to improve a patient’s lipid profile are suggested, along
with managing other risk factors. For patients with sufficiently high risk of cardiovascular disease, treatment with a statin is suggested. Secondary treatment with ezetimibe, with or without a PCSK9 inhibitor, may be considered in patients at very
high risk who have not had LDL-cholesterol reduction of 50% or more or who have LDL-cholesterol levels of 70 mg/dL or higher despite therapy with the maximum dose of a statin.
High-dose EPA has emerged as a new therapy to lower risk
of heart attack or stroke among patients taking a statin who have high triglyceride levels. Currently, new therapies in early clinical trials are showing promise and may change the way lipids are managed in the future given the trial outcomes.
Nicholas Fox and Nolan Fox are premedical students at Drexel University. Thomas Das, MD, is an Internal Medicine Physician on the Johns Hopkins Osler Medical Service. Roger S. Blumenthal, MD, FACC, is Director of the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease. Ethan Tumarkin, MD, is a postdoctoral fellow in the Johns Hopkins Division of Cardiology.